Nicotine’s Theoretical Protective Effects: Comparing Snake Venom Neurotoxins and COVID-19 Spike Proteins
- Randon Taylor

- Jul 10, 2025
- 13 min read
Updated: Jul 17, 2025

Nicotine, a compound synonymous with tobacco use, has long been a subject of scientific curiosity due to its interactions with nicotinic acetylcholine receptors (nAChRs). Beyond its role in addiction, nicotine’s pharmacological properties have sparked speculation about its potential to mitigate certain biological threats—including snake venom neurotoxins and, more recently, the spike proteins of SARS-CoV-2.
This article explores the theoretical protective effects of nicotine against bites from Chinese kraits (Bungarus multicinctus) and cobras (Naja species), compared to its potential role against circulating spike proteins from COVID-19. By examining binding mechanisms, receptor saturation dynamics, tissue targeting, pharmacokinetics, and chronic modulation, we aim to explore nicotine’s hypothetical efficacy across two very different classes of biological threat—grounding our analysis in neurobiology, toxinology, and emerging virology.
The Neurotoxic Threat of Snake Venom
—Understanding Snake Venom Neurotoxins
Chinese kraits and cobras, both elapid snakes, deliver venom packed with potent neurotoxins that target the neuromuscular junction, often leading to flaccid paralysis and death. These toxins act rapidly and with high specificity.
• Alpha-bungarotoxin (from kraits) binds irreversibly to muscle-type nAChRs, blocking acetylcholine and preventing muscle contraction (study)
• Alpha-cobratoxin (from cobras) behaves similarly, also targeting nAChRs with exceptionally high affinity—measured in the femtomolar to picomolar range (biochemical profile).
• Additional components such as beta-bungarotoxin act presynaptically, impairing neurotransmitter release (neurophysiology review).
These toxins cause rapid-onset weakness, ptosis, respiratory failure, and can be fatal if not treated with antivenom and respiratory support.
For a related breakdown on how nicotine may interact with different types of venom—specifically rattlesnake venom, which targets different receptor systems than cobra or krait neurotoxins—see my follow-up post: Nicotine vs. Rattlesnake Venom: Receptor Protection.

Nicotine’s Interaction with nAChRs
Nicotine, a plant alkaloid, is an agonist of multiple nAChR subtypes. Its most notable targets include:
• α4β2 (dominant in brain regions associated with addiction, attention, and arousal)
• α7, involved in memory, neuroprotection, and immune regulation, as demonstrated in this study.
• Muscle-type (α1β1δε/γ)—though nicotine binds this subtype with much lower affinity than neurotoxins.
By mimicking acetylcholine, nicotine activates these receptors, influencing neurotransmission, muscle tone, cognition, immune function, and autonomic balance. Peak nicotine levels from cigarette smoking (~30–50 ng/mL) translate to ~2 × 10⁻⁷ M in plasma—orders of magnitude lower than venom concentrations found at envenomation sites (nicotine pharmacokinetics).
Receptor Dynamics: Redundancy, Not Vulnerability
One simplistic critique of nicotine’s utility in venom defense is that it upregulates receptors—creating “more targets” for toxins. But this misrepresents how receptor dynamics work.
• Chronic nicotine exposure upregulates nAChRs, especially α4β2 and α7.
• This leads to receptor reserve: an expanded pool of receptors not required for baseline function.
• In this context, a fixed dose of venom must occupy more targets to induce the same degree of neuromuscular shutdown.
In experimental models, systems with upregulated receptors required 2–3x more toxin to cause equivalent inhibition. I’m other words 2–3× more venom is required to achieve equivalent paralysis in animals with nAChR upregulation (binding resistance study).
This creates a pharmacological buffer. Instead of increasing vulnerability, nicotine may increase resilience—particularly in systems where a small number of functional receptors can preserve life (e.g., diaphragm, brainstem, vagus nerve).
Rather than amplifying risk, nicotine-induced receptor redundancy may dilute venom impact—especially in critical systems like respiration or autonomic tone.
The Critical Systems That Matter Most
When survival is on the line, where nicotine acts is more important than whether it reaches the bite site.
Venom is delivered locally and overwhelms receptors at the site of injection. But paralysis of an arm or leg is survivable. Paralysis of the diaphragm or medullary centers is not.
Nicotine concentrates in the brain, lungs, and adrenal glands, influencing:
• Phrenic nerve signaling (diaphragm control)
• Medullary respiratory centers
• Cardiac autonomic regulation
• Adrenal medulla and sympathetic tone
If nicotine preserves cholinergic signaling in these regions—even partially—it may delay systemic collapse long enough for mechanical ventilation or antivenom administration.

The Limits of Competition: Why Nicotine Alone May Not Prevent Acute Envenomation
Despite its systemic effects, nicotine faces formidable limitations in the context of acute snakebite:
• Alpha-bungarotoxin and alpha-cobratoxin bind ~10,000x more tightly than nicotine at nAChRs (affinity study)
• Venom is delivered in a high-concentration bolus, rapidly saturating receptors at the bite site.
• Nicotine, by contrast, is systemic and diffuse, and cannot achieve comparable local concentrations in time.
Snake venom neurotoxins such as α-bungarotoxin bind to nicotinic acetylcholine receptors with nanomolar affinity, whereas nicotine’s affinity is in the micromolar range, making it approximately 3,400 times less potent in receptor binding.
Even if nicotine is preloaded, the venom acts too quickly and binds too tightly to be displaced.
However, this does not mean theoretical protection is zero.
Estimated systemic protective effect: ~10–30% under ideal conditions, if vital systems are spared or if functional receptor pools delay total collapse.

Timeline Matters: Burst vs. Wave
Venom is a single-use weapon. It strikes fast, hits hard, and depends on localized action.
Nicotine is a wave—sustained, repeatable, and adaptable:
• It can be administered through patches, gum, lozenges, or nebulization.
• Blood levels can be maintained or boosted post-bite.
• This allows longer-term receptor support even as venom damage unfolds.
Additionally, nicotine may play a role in post-acute recovery by supporting cholinergic tone, reducing inflammation, and promoting receptor re-expression in surviving neurons.
The Spike Protein Hypothesis: A New Kind of Neurotoxin
Mechanism of Action
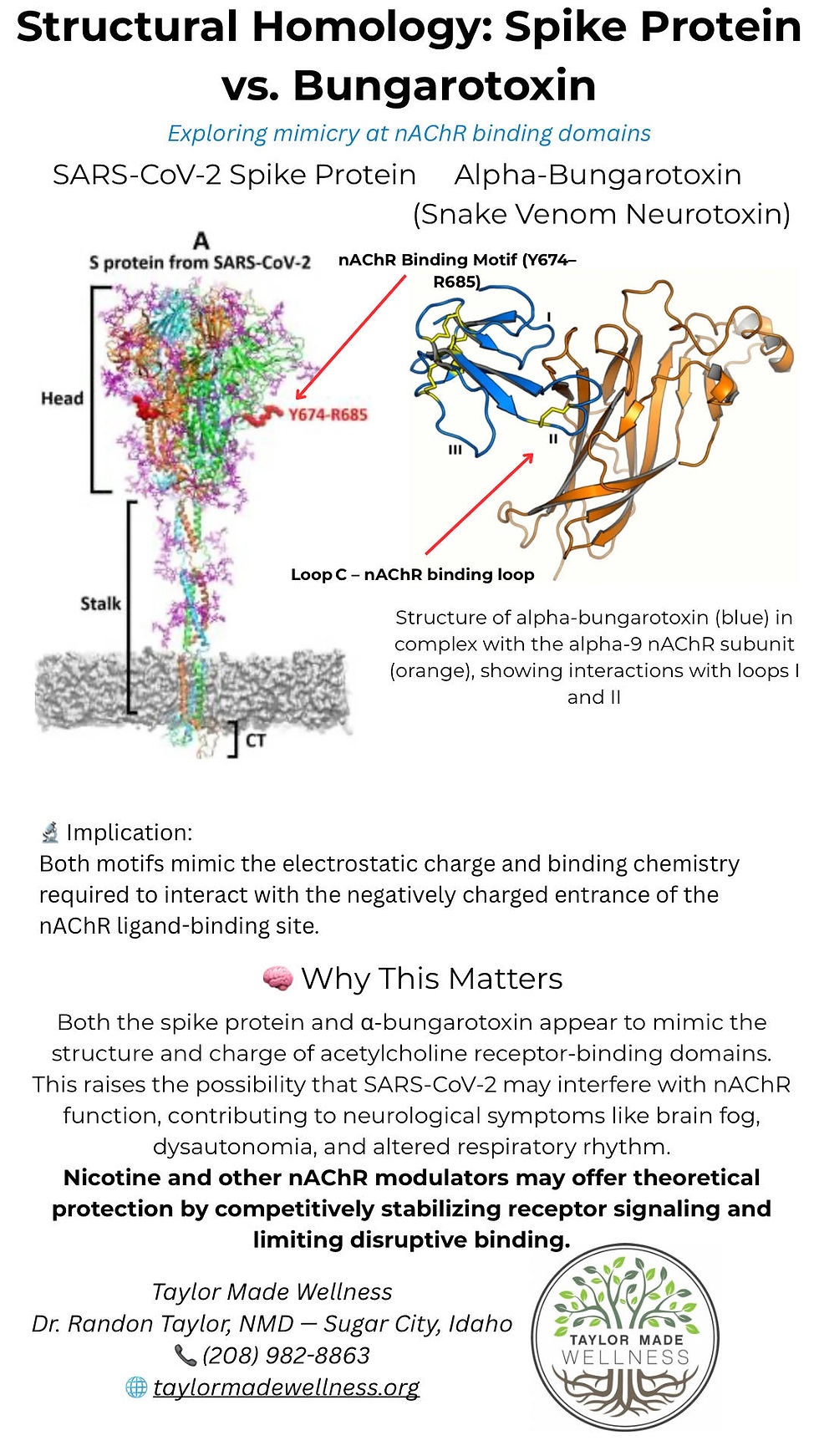
SARS-CoV-2 spike proteins bind to ACE2 receptors to enter cells—but computer modeling (in silico studies) suggests that certain segments of the spike protein may also bind nicotinic acetylcholine receptors (nAChRs), particularly the α7 and α4β2 subtypes, due to shared structural motifs with snake neurotoxins like alpha-bungarotoxin.
While the SARS-CoV-2 spike protein primarily binds to ACE2 receptors to facilitate viral entry, computational studies suggest that its Y674–R685 region may also interact with α7 and α4β2 nicotinic acetylcholine receptors, potentially impacting cholinergic signaling pathways.
Unlike venom, spike proteins:
• Are systemic rather than localized
• Operate over days to weeks, not seconds
• May cause chronic modulation, not outright blockade
Spike protein fragments have been detected in plasma for up to 28 days following mRNA vaccination, particularly in myocarditis cases, and in lymph nodes up to 60 days post-vaccination. Additionally, persistent spike protein has been identified in monocytes up to 15 months after infection, suggesting longer-term antigen presence beyond typical serum detection windows. A separate proteomics analysis also detected spike-derived peptides in circulation as late as 69 and 187 days post-vaccination.
The Chimera Concept: Venom Motifs Hidden in the Virus
Computational analyses have revealed regions of homology between spike proteins and snake venom peptides.
• Motifs resembling alpha-bungarotoxin and cobratoxin have been identified in spike protein structures (study).
• These may mimic or interfere with nAChR function, especially in autonomic and inflammatory circuits.
This raises the hypothesis that COVID-19 and spike-related syndromes may resemble a slow-motion neurotoxic envenomation.
This could explain:
• Long COVID symptoms like fatigue, POTS, brain fog, and dysautonomia
• Post-vaccine syndromes with tachycardia, adrenal instability, and neurological events
• Chronic immune dysfunction via α7 nAChR suppression
Although the SARS-CoV-2 spike protein and alpha-bungarotoxin differ in overall structure and origin, both contain highly similar binding motifs—short sequences with nearly identical charge, shape, and spatial presentation. The spike’s Y674–R685 loop, especially with its unique PRRA insert, mirrors the electrostatic profile and receptor-targeting geometry of bungarotoxin’s loop C, which is known to bind the nicotinic acetylcholine receptor (nAChR). These aren’t just generic resemblances; they’re precisely positioned “teeth on a key” that may allow both proteins to fit the same molecular lock. This functional mimicry suggests the spike protein may hijack nAChR pathways in a toxin-like manner—engaging the same aromatic residues and triggering similar downstream effects, despite being a structurally unrelated viral glycoprotein.
Long COVID has introduced a wide spectrum of symptoms—many of which point to autonomic and cholinergic disruption: fatigue, brain fog, POTS, shortness of breath, and altered smell or taste. These aren’t random—they suggest that spike protein may continue interfering with nicotinic acetylcholine receptors (nAChRs) long after the initial infection clears. In that context, nicotine’s ability to bind and stabilize these receptors may explain why some long COVID patients report improvements with low-dose, cyclic use. Whether through direct receptor modulation or by restoring balance in the cholinergic anti-inflammatory pathway, nicotine may help reestablish function in systems that have been stuck in a dysregulated loop. From what I’ve seen in my own case—and in my family—the deeper and longer the disruption, the more gradual the recovery. But the pattern is real.
🧠 Summary: How This Supports the Hypothesis
Feature | Spike (YQTQTNSPRRAR) | Bungarotoxin (Loop C) | Shared Implication |
Rich in Arg (R) | ✅ RRAR | ✅ R, H | Strong positive charge → binds nAChR |
Flexible loop region | ✅ Exposed binding loop | ✅ Loop C | Can fit into ligand pocket of receptor |
Binds nAChRs | Theoretical disruption | Established blockade | Same receptor target → functional mimicry |
Clinical effect | Neurological + respiratory | Paralysis + neurotoxicity | nAChR-linked system disruption |
Nicotine as a Functional Antidote to Spike Protein Damage?
In contrast to its failure in acute venom competition, nicotine may offer functional protection in the slow-burning context of spike exposure.
1. Cholinergic Anti-Inflammatory Pathway
Nicotine activates α7 nAChRs on immune cells, reducing IL-6, TNF-α, and other cytokines—buffering systemic inflammation (study).
2. Receptor Preservation
Recent research suggests that a specific segment of the SARS-CoV-2 spike protein may bind to and impair α7 nAChRs—similar to how some snake venom toxins work.
A study in Molecular Neurobiology found that this region of the spike protein can act like a non-competitive antagonist, reducing the receptor’s activity and potentially disrupting autonomic and immune signaling.
Because nicotine is a known α7 nAChR agonist, it may help offset this disruption by keeping these receptors active and functional.
3. Autonomic Stabilization
Nicotine modulates vagal tone, helping normalize HRV, blood pressure, and digestive motility—all commonly disrupted in spike-related syndromes.
4. Tissue Selectivity
Nicotine reaches lungs, CNS, adrenal medulla, and lymphoid tissue—the same regions where spike proteins tend to concentrate.
Reframing the Comparison: Fast Shock vs. Slow Disruption
Parameter | Snake Venom | COVID-19 Spike Protein |
Delivery | Local injection | Systemic circulation |
Timeline | Seconds to minutes | Days to weeks |
Receptor Target | Muscle-type nAChRs | ACE2 + neuronal nAChRs |
Mechanism | Irreversible blockade | Modulation, desensitization |
System Failure | Respiratory, neuromuscular | Autonomic, inflammatory, cognitive |
Nicotine Role | Weak competitor | Functional modulator |
Protection Estimate | ~10–30% (ideal cases) | ~30–60% (context-dependent) |

Additional Considerations: The Edge Few Discuss
• Genetics: CYP2A6 slow metabolizers retain nicotine longer—possibly offering more prolonged protection. Some individuals also overexpress α7 or α4β2 receptors, which may shift outcomes dramatically.
• Neuroplasticity: Nicotine promotes receptor recycling, glial buffering, and synaptic repair—potentially aiding in recovery after spike or venom insult.
• Oxidative Stress: Low-dose nicotine reduces ROS and enhances mitochondrial efficiency, possibly mitigating toxin-induced apoptosis.
• Endocrine Resilience: Nicotine’s effects on the adrenal medulla may stabilize catecholamine output, buffering shock or dysautonomia.
Personal Observations on Nicotine’s Effects
This isn’t abstract for me—it changed everything. COVID didn’t just disrupt life; it left lasting marks. I still think about my dad. I miss him.
After COVID, I was stuck with a lung symptom that never fully went away—constant mucus I had to clear from my throat all day. It had been going on for over two years. The most annoying was at night. I’d wake up multiple times, sometimes loud enough to wake my wife, just clearing my throat over and over.
What finally changed things was nicotine.
I started using it after hearing what it had done for family. Once I dug into the science, the theory made sense—nicotine binds to nicotinic acetylcholine receptors (nAChRs), the same ones spike protein is believed to interfere with. Within a couple of months on microdosing, the mucus was gone. I can’t even describe how annoying it was to be clearing my throat all the time.
But if I went too long without nicotine—three or four days or more—it came back. Not fully, but noticeably. I’ve always cycled off regularly, usually 1–2 times per month, but I now keep those breaks shorter so the symptom doesn’t return. I’ve used nicotine like this for over six months with zero signs of dependence:
No cravings
No withdrawal
No irritability
No mental drop
No compulsion whatsoever
That’s important to say—because for all the concern about nicotine addiction, dose, delivery method, and cycling seem to matter just as much. When used intentionally and in micro amounts, I’ve experienced none of the hallmarks of dependence.
My family’s anecdotal experience has been interesting as well—I come from a large family.
My sister had completely lost her sense of taste after COVID—everything tasted off, but one thing in particular lingered: peanut butter tasted horrible, even a year later. That was the last taste distortion to resolve. After starting nicotine, it finally reset. She can eat it normally now. “It brought back some of my loss of taste and smell like peanut butter, the smell of coffee. Also I felt my lungs were weak after getting Covid and the jab. I got really sick back in October with mucus in my lungs and a really bad cough, it went on for weeks and I wasn't getting better. I finally had to get on a Z-Pack from the Dr to get rid of it. I felt weak after too. I started the nicotine around November, I think, since then I have felt great, my lungs have felt great and I haven't gotten sick at all! Even when my kids were sick around me. It's definitely helped my immune system. I still take 6mg a day but about once a month I take a break from it for a week.”
My 22 year old son lost 100% of his sense of smell and taste during COVID. It took over a month, but both returned completely after low-dose nicotine. In his case, I believe youth and overall health played a big role in the speed of recovery.
In my opinion, the more severe the sensory disruption, the more often you've experienced COVID—and the longer it’s been present—the longer it will take to restore. Especially if, like me, you’ve had COVID multiple times with pronounced symptoms. I had it twice with significant loss of taste and smell both times. These aren’t just minor symptoms—they’re signs that the cholinergic nervous system has been hijacked, and that system doesn’t bounce back overnight.
Recovery seems to scale with both severity and duration. A subtle case might resolve in weeks. A deeply embedded symptom, like mine, takes much longer. And if you've had COVID more than once, expect it to take time.
I’m not making clinical claims. But I’ve lived the theory. And for me, nicotine—when used carefully and deliberately—has done what nothing else could.
Conclusion: Context is Everything
Nicotine is not an antivenom. It is not an antiviral. But it may be a neuromodulatory stabilizer with unexpected utility.
• In snakebite, nicotine is overwhelmed by sheer binding kinetics and local venom concentration—but may still delay collapse by preserving autonomic signaling elsewhere.
• In spike protein exposure, nicotine may counteract chronic nAChR suppression, rebalance autonomic tone, and reduce inflammation—making it a plausible therapeutic adjunct.
Nicotine isn’t trying to beat the venom. It’s trying to outlast the toxin.
Further research is needed, but the convergence of toxinology, virology, and receptor pharmacology paints an intriguing picture: a simple alkaloid, misunderstood and maligned, may hold a key to both acute resilience and chronic recovery—from long COVID.
If you're curious about how to approach nicotine safely—especially for microdosing, cycling, or long COVID recovery support—I’ve put together a free guide outlining practical nicotine dosing strategies, cycling schedules, and delivery methods. You can download it here: Nicotine Dosing Guidelines: Microdosing, Cycling, and Receptor Targeting
Disclaimer:
This article is for educational and informational purposes only. It is not intended to diagnose, treat, or prevent any disease or condition. The theoretical mechanisms discussed are based on emerging scientific hypotheses and are not a substitute for professional medical advice. Always consult a licensed healthcare provider for medical guidance, especially in the case of snakebite, envenomation, or COVID-19 complications.
About the Author:
Dr. Randon Taylor, NMD is a licensed naturopathic medical doctor and founder of Taylor Made Wellness in Sugar City, Idaho. With clinical expertise in integrative medicine, toxicology, and neuroimmune health, he specializes in complex chronic illness, genetic analysis, and detoxification protocols. Dr. Taylor draws on both research and hands-on experience to explore emerging therapeutic strategies with practical relevance.
Author’s Note:
This article represents the culmination of six months of research, synthesis, and critical thinking. When I first set out to understand whether nicotine could offer any protection against snake venom or spike proteins, I found nothing—no direct data, no clear pathways, just speculation and dismissal. It wasn’t until I started thinking outside the framework of conventional pharmacology and began exploring chimera toxin structures, receptor redundancy, and chronic signaling disruption, that the patterns began to emerge.
What started as a question about venom evolved into a broader investigation of how biology uses similar tools for very different purposes—and how molecules like nicotine, long misunderstood, might have unexpected roles in modulating our response to those tools.
This is not a claim of certainty—but a map of possibilities. I share it here in the hope that it opens new questions for researchers, clinicians, and critical thinkers alike.
—Dr. Randon Taylor
Published: July 10, 2025
Note: This article is a theoretical exploration based on emerging research. It does not recommend nicotine use for medical purposes, as its risks, particularly through smoking, are well-documented. Readers should consult with qualified health professionals for diagnosis and treatment.
References
Chang, C.C. Looking back on the discovery of alpha-bungarotoxin. Journal of Biomedical Science.
Barber, C.M. et al. Alpha-cobratoxin and related toxins: structure and function. Toxicon.
Albuquerque, E.X. et al. Mammalian nicotinic acetylcholine receptors: from structure to function. Physiological Reviews.
Benowitz, N.L. Pharmacokinetic considerations in understanding nicotine dependence. Ciba Foundation Symposium.
Hukkanen, J. et al. Metabolism and disposition kinetics of nicotine. Pharmacological Reviews.
Wonnacott, S. The paradox of nicotinic acetylcholine receptor upregulation by nicotine. Trends in Pharmacological Sciences.
Levandoski, M.J. et al. Competitive antagonism of alpha-bungarotoxin by nicotine. Biochemical Pharmacology.
Warrell, D.A. Snake bite. Lancet.
Hoffmann, M. et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2. Cell.
Changeux, J.P. et al. A nicotinic hypothesis for Covid-19. Comptes Rendus Biologies.
Ogata, A.F. et al. Circulating SARS-CoV-2 vaccine antigen detected in plasma. Clinical Infectious Diseases.
Wang, H. et al. Nicotinic acetylcholine receptor alpha7 subunit regulates inflammation. Nature.
Leung, J.M. et al. COVID-19 and nicotine as a mediator of ACE2. European Respiratory Journal.
Farsalinos, K. et al. Review of smoking prevalence among COVID-19 patients. Internal and Emergency Medicine.
Miyara, M. et al. Low incidence of smoking in symptomatic COVID-19 patients. Qeios.
Simons, D. et al. Smoking status and SARS-CoV-2 infection: a rapid review. Addiction.
Brake, S.J. et al. Smoking upregulates ACE2 receptor. Journal of Clinical Medicine.
WHO. Smoking and COVID-19: Scientific brief.



Comments